Introduction
Dry eye syndrome involves insufficient lubrication and moisture on the eye’s surface, affecting tear production or quality. This overview examines evidence-based approaches for managing and preventing this common ocular condition.
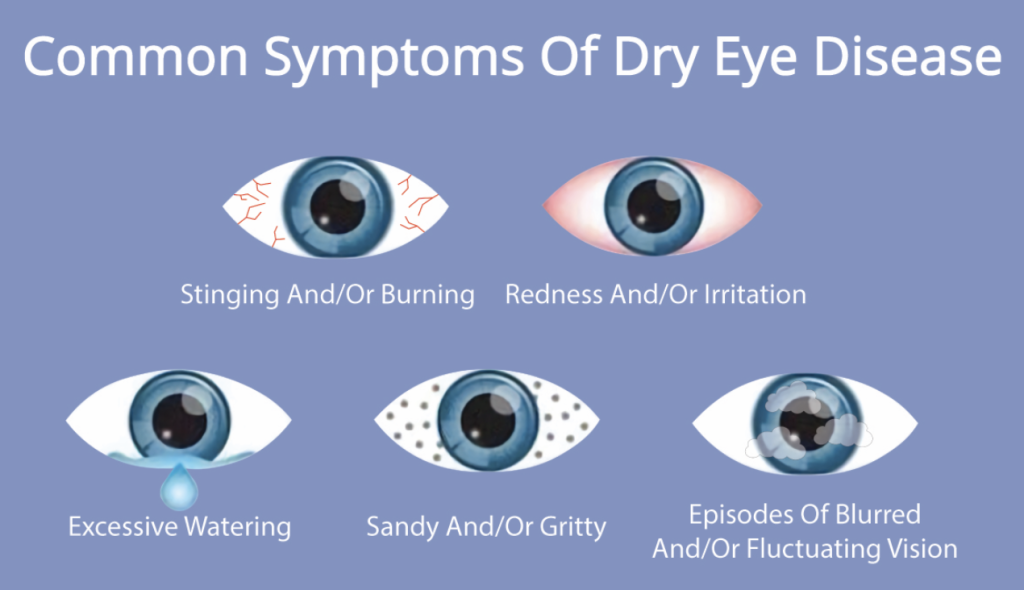
Primary Symptoms
- Persistent dryness and irritation
- Redness and inflammation
- Blurred vision that improves with blinking
- Sensitivity to light
- Foreign body sensation
Common Contributing Factors
- Aging-related tear production changes
- Screen use and reduced blinking rate
- Environmental factors (low humidity, wind)
- Certain medications and health conditions
- Contact lens wear
Professional Diagnosis
- Comprehensive eye examination
- Tear quality and quantity assessment
- Tear breakup time measurement
- Ocular surface evaluation
- Identification of underlying causes
Treatment Approaches
- Preservative-free artificial tears
- Anti-inflammatory eye drops
- Punctal occlusion procedures
- Environmental modification strategies
- Eyelid hygiene protocols
Prevention
Preventing dry eye syndrome requires scientifically supported protective measures. Experts recommend maintaining regular breaks from screen use, following the 20-20-20 rule (looking at something 20 feet away for 20 seconds every 20 minutes). Proper eyelid hygiene, including regular cleaning of the eyelash base, helps maintain normal meibomian gland function. Using humidifiers in dry environments or wearing protective glasses in dusty conditions can reduce environmental triggers. A balanced diet with adequate Omega-3 fatty acids may support ocular health. Individuals experiencing persistent eye discomfort should consult qualified ophthalmologists for personalized advice. The effectiveness of these measures may vary depending on individual circumstances.
Lifestyle Modifications
- Regular blinking exercises during screen use
- Environmental humidity maintenance
- Protective eyewear in windy conditions
- Adequate hydration and nutritional support
- Proper contact lens hygiene practices
Medical Interventions
- Lubricating eye drops and ointments
- Prescription anti-inflammatory medications
- In-office procedures for tear conservation
- Thermal expression of meibomian glands
- Autologous serum eye drops (severe cases)
When to Seek Professional Care
- Persistent symptoms despite self-care
- Significant pain or visual changes
- Inability to perform daily activities
- Symptoms following ocular surgery
- Association with autoimmune conditions
Prevention Strategies
- Regular comprehensive eye examinations
- Conscious blinking during digital device use
- Avoidance of direct air currents from fans
- Nutritional support with omega-3 fatty acids
- Proper management of underlying health conditions
Conclusion
Dry eye management requires professional diagnosis to develop effective, individualized treatment plans. Evidence-based approaches combine lifestyle modifications with medical interventions to improve ocular surface health and patient comfort. Regular follow-up care ensures appropriate adjustment of treatment strategies based on symptom progression and treatment response.